Source – https://phys.org/
Small-molecule therapeutics treat a wide variety of diseases, but their effectiveness is often diminished because of their pharmacokinetics—what the body does to a drug. After administration, the body dictates how much of the drug is absorbed, which organs the drug enters, and how quickly the body metabolizes and excretes the drug again.
Nanoparticles, usually made out of lipids, polymers, or both, can improve the pharmacokinetics, but they can be complex to produce and often carry very little of the drug.
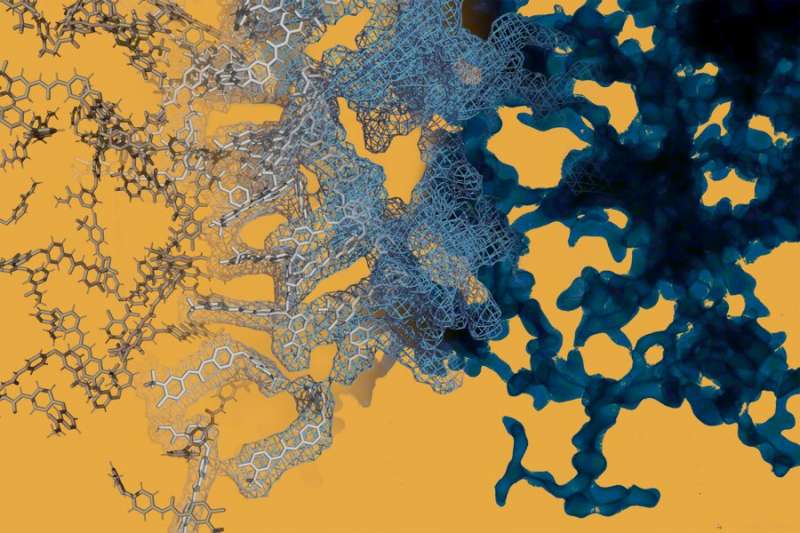
Some combinations of small-molecule cancer drugs and two small-molecule dyes have been shown to self-assemble into nanoparticles with extremely high payloads of drugs, but it is difficult to predict which small-molecule partners will form nanoparticles among the millions of possible pairings.
MIT researchers have developed a screening platform that combines machine learning with high-throughput experimentation to identify self-assembling nanoparticles quickly. In a study published in Nature Nanotechnology, researchers screened 2.1 million pairings of small-molecule drugs and “inactive” drug ingredients, identifying 100 new nanoparticles with potential applications that include the treatment of cancer, asthma, malaria, and viral and fungal infections.
“We have previously described some of the negative and positive effects that inactive ingredients can have on drugs, and here, through a concerted collaboration across our laboratories and core facilities, describe an approach focusing on the potential positive effects these can have on nanoformulation,” says Giovanni Traverso, the Karl Van Tassel (1925) Career Development Professor of Mechanical Engineering, and senior corresponding author of the study.
Their findings point to a strategy for that solves for both the complexity of producing nanoparticles and the difficulty of loading large amounts of drugs onto them.
“So many drugs out there don’t live up to their full potential because of insufficient targeting, low bioavailability, or rapid drug metabolism,” says Daniel Reker, lead author of the study and a former postdoc in the laboratory of Robert Langer. “By working at the interface of data science, machine learning, and drug delivery, our hope is to rapidly expand our tool set for making sure a drug gets to the place it needs to be and can actually treat and help a human being.”
Langer, the David H. Koch Institute Professor at MIT and a member of the Koch Institute for Integrative Cancer Research, is also a senior author of the paper.
A cancer therapy meets its match
In order to develop a machine learning algorithm capable of identifying self-assembling nanoparticles, researchers first needed to build a dataset on which the algorithm could train. They selected 16 self-aggregating small-molecule drugs with a variety of chemical structures and therapeutic applications and a diverse set of 90 widely available compounds, including ingredients that are already added to drugs to make them taste better, last longer, or make them more stable. Because both the drugs and the inactive ingredients are already FDA-approved, the resulting nanoparticles are likely to be safer and move through the FDA approval process more quickly.
The team then tested every combination of small-molecule drug and inactive ingredient, enabled by the Swanson Biotechnology Center, a suite of core facilities providing advanced technical services within the Koch Institute. After mixing pairings and loading 384 samples at a time onto nanowell plates using robotics in the High Throughput Sciences core, researchers walked the plates, often with quickly degrading samples, next door to the Peterson (1957) Nanotechnology Materials Core Facility core to measure the size of particles with high throughput dynamic light scattering.
Now trained on 1,440 data points (with 94 nanoparticles already identified), the machine learning platform could be turned on a much bigger library of compounds. Screening 788 small-molecule drugs against more than 2,600 inactive drug ingredients, the platform identified 38,464 potential self-assembling nanoparticles from 2.1 million possible combinations.
The researchers selected six nanoparticles for further validation, including one composed of sorafenib, a treatment commonly used for advanced liver and other cancers, and glycyrrhizin, a compound frequently used as both a food and drug additive and most commonly known as licorice flavoring. Although sorafenib is the standard of care for advanced liver cancer, its effectiveness is limited.
In human liver cancer cell cultures, the sorafenib-glycyrrhizin nanoparticles worked twice as well as sorafenib by itself because more of the drug could enter the cells. Working with the Preclinical Modeling, Imaging and Testing facility at the Koch Institute, researchers treated mouse models of liver cancer to compare the effects of sorafenib-glycyrrhizin nanoparticles versus either compound by itself. They found that the nanoparticle significantly reduced levels of a marker associated with liver cancer progression compared to mice given sorafenib alone, and lived longer than mice given sorafenib or glycyrrhizin alone. The sorafenib-glycyrrhizin nanoparticle also showed improved targeting to the liver when compared to oral delivery of sorafenib, the current standard in the clinic, or when injecting sorafenib after it has been combined with cremophor, a commonly-used drug vehicle that improves water solubility but has toxic side effects.
Personalized drug delivery
The new platform may have useful applications beyond optimizing the efficiency of active drugs: it could be used to customize inactive compounds to suit the needs of individual patients. In earlier work, members of the team found that inactive ingredients could provoke adverse allergic reactions in some patients. Now, with the expanded machine learning toolbox, more options could be generated to provide alternatives for these patients.
“We have an opportunity to think about matching the delivery system to the patient,” explains Reker, now an assistant professor of biomedical engineering at Duke University. “We can account for things like drug absorption, genetics, even allergies to reduce side effects upon delivery. Whatever the mutation or medical condition, the right drug is only the right drug if it actually works for the patient.”
The tools for safe, efficacious drug delivery exist, but putting all the ingredients together can be a slow process. The combination of machine learning, rapid screening, and the ability to predict interactions among different combinations of materials will accelerate the design of drugs and the nanoparticles used to deliver them throughout the body.
In ongoing work, the team is looking not just to improve effective delivery of drugs but also for opportunities to create medications for people for whom standard formulations are not a good option, using big data to solve problems in small populations by looking at genetic history, allergies, and food reactions.